Introduction
- Problem: Many people rely on wearable devices to gauge how they move, how hard their heart works, and even how well they sleep. But uncertainty remains: are these trackers truly accurate, and do they meaningfully improve health?
- Agitation: Without trustworthy guidance, users risk chasing numbers that don’t reflect reality, misinterpreting data, or feeling frustrated when enthusiasm fades and results stall.
- Solution: This article distills the best available evidence and our clinical experience to explain what trackers measure, how accurate they are, what health benefits we can reasonably expect, and how to use them as a practical, anxiety-reducing tool. By the end, you’ll know exactly how to get value from wearables without chasing false certainty. Read on to uncover the science behind the signals and how to apply it in your daily routine.
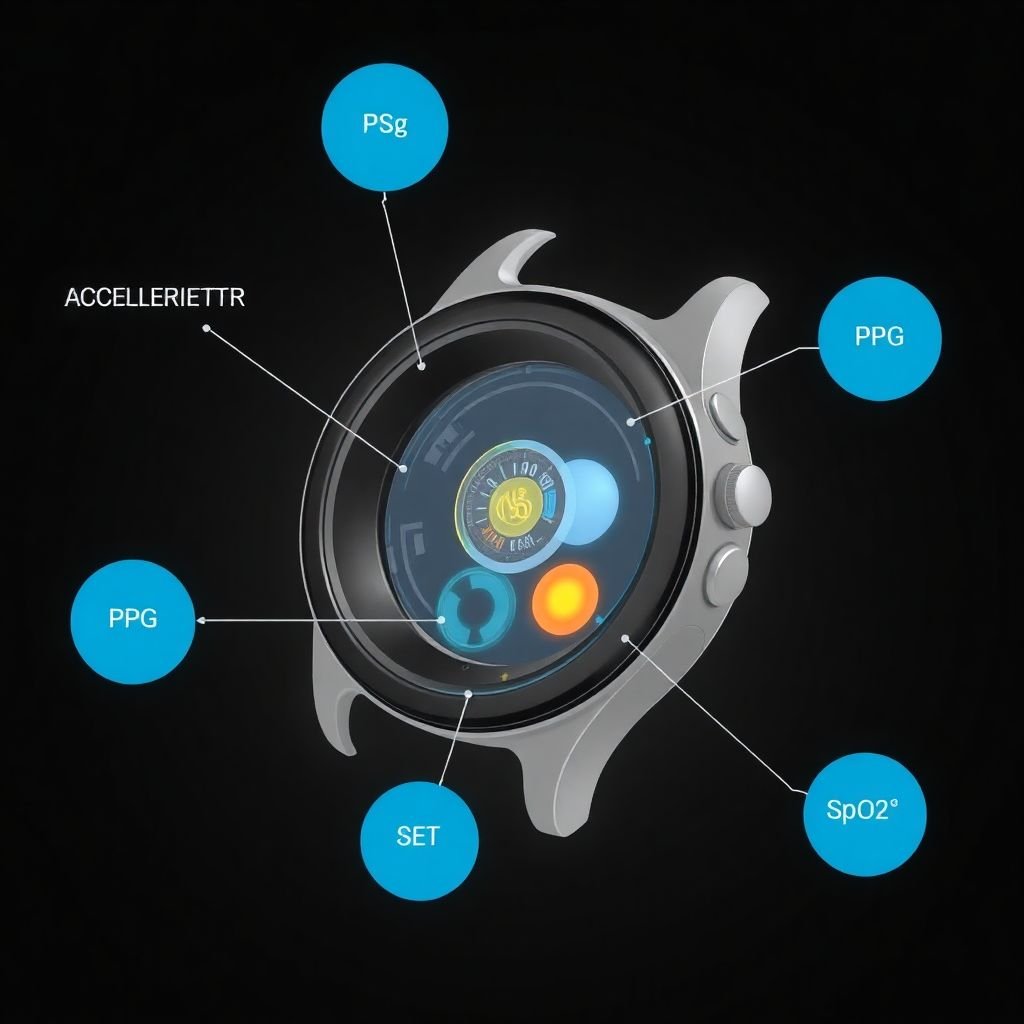
What Do Fitness Trackers Measure? Wearable devices come in many shapes and styles, but at their core they share a common purpose: to quantify movement and physiological signals so you can interpret your daily performance and trends.
- Movement and steps: Most trackers use a motion sensor (accelerometer) to count steps and estimate activity level.
- Heart rate: A photoplethysmography (PPG) sensor tracks heart rate, providing resting rates and real-time estimates during activities.
- Energy expenditure: Calorie burn estimates combine movement data with basic personal details (height, weight, sex, age) to approximate how many calories you’re using.
- Blood oxygen level (SpO2): Many modern wearables include SpO2 sensing, useful for certain health contexts and wellness monitoring.
- Sleep patterns: Some devices track sleep duration and stages using movement and, in newer models, more advanced algorithms.
Key nuance: devices vary in what they measure and how they interpret signals. In our clinical experience, this matters when you compare across devices or rely on one device for long-term decisions.
How Accurate Are They? The accuracy story is nuanced and depends on what you’re measuring, the context, and the device itself.
- Steps: Trackers are generally pretty good at counting steps and are often about as accurate as research-grade pedometers. Caveat: very slow walking or unusual gait can lead to undercounting, while lots of hand movement can overcount.
- Heart rate: Resting heart rate measurements tend to be quite reliable. During exercise, accuracy can dip and vary by device. In our experience, newer devices with multiple data inputs often perform better, but no wrist-worn monitor matches a clinical-grade monitor in all scenarios.
- Energy expenditure (calorie burn): This is the area with the most variability. Calorie burn estimates rely on algorithms that combine movement data with personal characteristics and, sometimes, heart rate. Most trackers underestimate burn during certain activities (e.g., cycling or workouts with limited wrist movement) and accuracy can differ widely by device. Some of the latest sensors that fuse motion, heart rate, and other data improve estimates, but they still aren’t a perfect measure of actual energy expenditure.
- Blood oxygen (SpO2): Wrist-based SpO2 readings are reasonably close to clinical pulse oximeters in many contexts but are not a substitute for medical devices when precise oxygen measurements are needed. They can be helpful for home monitoring, but accuracy can vary by device and usage conditions.
- Sleep tracking: Sleep stage classification is improving with newer hardware and algorithms, but readability varies. It’s helpful for trends, not a precise medical assessment.
In our clinical experience, device choice matters. A common mistake we observe is assuming all trackers are interchangeable or treating data from one device as definitive medical evidence. The reality is that accuracy is device- and context-dependent, and the best use of wearables is as a signal in a broader health picture.
The Research: Do They Improve Health? A big question remains: even if trackers are imperfect, do they help people become healthier?
- Early findings showed modest or inconsistent effects. In several initial studies, people with trackers were slightly more active than those without, but overall fitness and health markers often showed little change.
- Adherence is a major driver. A sizable share of users discontinue tracking within the first six months, which undermines long-term benefits. It’s a lot like a gym membership: motivation can spike, but persistence requires clear value and support.
- When trackers are integrated with guided programs, results improve. In some studies that added exercise prescriptions, dietary guidance, and counseling, trackers did not automatically boost activity. However, when users maintained engagement and combined tracking with actionable coaching, benefits tended to be stronger.
On balance, the most robust synthesis to date suggests modest health effects across large populations:
- Activity: around an additional 1,800 steps per day on average, or about 40 more minutes of walking daily.
- Weight: modest weight loss, typically around 2 pounds on average.
- Cardiometabolic markers: improvements in blood pressure and cholesterol have been observed, particularly among individuals with chronic conditions who stay engaged with the devices and accompanying guidance.
What this Means in Practice
- The news is not zero or nothing. Trackers provide useful behavioral nudges and immediate feedback, which can support healthier choices when used thoughtfully.
- The biggest payoff comes when tracking is paired with clear goals, structured activity plans, and ongoing motivation—rather than as a standalone solution.
- For people with chronic diseases, wearables can help monitor trends and support routine management when used with professional guidance.
In our experience, wearables are less about precision medicine and more about ongoing, data-informed behavior change. They are starting to function as practical health trackers, and the potential to support diagnosis and management with AI is growing—but that future requires careful validation and regulation.
The Future: From Monitoring to Diagnosing Device makers are pushing beyond tracking toward diagnostic capabilities. Some notable trends include:
- Atrial fibrillation monitoring: Smartwatches are increasingly able to detect abnormal heart rhythms with reasonable reliability, which can prompt medical evaluation.
- Sleep analytics: Sleep-time measurement is improving, with ring devices applying machine learning to classify sleep stages with greater nuance.
- Data synthesis: As sensors improve, artificial intelligence will help extract meaningful conclusions from vast streams of wearable data, aiding clinicians in diagnosis and management.
Bottom line: wearables are evolving from simple activity meters into potentially powerful health tools. In the coming years, they are likely to become a standard part of a clinician’s toolkit for certain conditions, while remaining valuable to the general public for everyday wellness.
Practical Guidelines: How to Use Wearables Effectively
- Set realistic goals and expectations. Use trackers to inform your routine, not to seek perfection.
- Focus on trends, not single days. Small day-to-day fluctuations are less informative than long-term trajectories.
- Combine data with context. Pair step counts or heart rate data with sleep quality, nutrition, stress management, and physical activity variety.
- Calibrate and customize. Use device-specific features (e.g., resting heart rate baseline, oxygen saturation alerts) in ways that fit your health context.
- Seek professional guidance when needed. Share relevant wearable data with your clinician to support decision-making.
- Protect your privacy. Understand what data your device collects and how it’s stored and shared.
Bucket Brigades to Keep Readers Engaged
- Sound familiar? You’re not alone in wondering if the data truly matter.
- Here’s the deal: trackers offer signals, not prescriptions.
- But that’s not all: future sensors and AI will help turn raw signals into actionable insights.
- In our clinical experience, the most reliable path is pairing data with coaching and a clear plan.
YMYL Note: Health information requires care Because this topic touches health, we avoid definitive medical prescriptions. Always consult a healthcare professional for diagnosis or treatment decisions. Use wearables as tools to inform conversations with your clinician, not as substitutes for professional care.
Conclusion: The Big Idea Revisited Wearable fitness trackers have progressed from simple pedometers to sophisticated health signals. They offer reliable steps data and useful heart-rate trends, with reasonable methods to monitor oxygen saturation and sleep, while calorie-burn estimates remain the trickiest area. Importantly, the strongest health benefits arise when trackers are used consistently in conjunction with clear goals, coaching, and context—not as standalone magic bullets.
- Recap of the core insight: Trackers provide valuable signals that can support healthier behavior when used thoughtfully and in combination with professional guidance.
- The transformation: From basic activity monitors to potential health trackers that assist diagnosis and management—reflecting the evolving role of wearables in healthcare.
- Big idea: The true value of wearables lies in sustained, informed action—data plus guidance equal progress.
Ready to reclaim your health with wearable tracking? Take the first step and explore our free, no-commitment resources to turn signals into sustainable results.
